La neurociencia más allá de las neuronas
- Borrajo, A.; Spuch, C.; Penedo; M.A.; Olivares, J.M.; Agís-Balboa, R.C. (2021) Important role of microglia in HIV-1 associated neurocognitive disorders and the molecular pathways implicated in its pathogenesis. Annals of Medicine, 53(1). pp:43-69 | doi: 1080/07853890.2020.1814962
- Carvalho da Fonseca, A.C.; Amaral, R.; Garcia, C. & col. (2016)Microglia in Cancer: For Good or for Bad?. Advances in experimental medicine and biology, 949. pp: 245-261 | doi: 10.1007/978-3-319-40764-7_12.
- Jaen Manzanera, A. (2014) Trastornos neurocognitivos en personas con VIH +. Monográfico 2014. Revista Multidisciplinar del SIDA, 1(3). pp: 33-42.
- Undabeitia, J.; Torres-Bayona, S.; Samprón, N. & col. (2018) Costes indirectos asociados al glioblastoma. Experiencia en un centro. Neurología, 33(2). pp: 85-91 | doi: 1016/j.nrl.2016.05.003
- Río-Hortega, J. (2013) A propósito de los descubrimientos de la microglía y la oligodendroglía: Pío del Río-Hortega y su relación con Achúcarro y Cajal (1914-1934). Neurosciences and History, 1(4). pp: 176-190.
- Y, H.; Fryatt, G.L.; Ghorbani, M.; Obst, J. & col. (2021) Replicative senescence dictates the emergence of disease-associated microglia and contributes to Aβ pathology. Cell Reports, 35(10): 109228 | doi: 1016/j.celrep.2021.109228.
- Leng, F.; Edison, P. (2021) Neuroinflammation and microglial activation in Alzheimer disease: where do we go from here? Nature Reviews Neurology, 17(3). pp: 157-172 | doi: 1038/s41582-020-00435-y
- Hajji, N.; García-Revilla, J.; Sarmiento Soto, M. & col. (2022) Arginine deprivation alters microglial polarity and synergizes with radiation to eradicate non-arginine-auxotrophic glioblastoma tumors. The Journal of Clinical Investigation, 132(8): e142137 | doi: 1172/JCI142137
- Douglas Fields, R. (2008) Oligodendrocytes Changing the Rules: Action Potentials in Glia and Oligodendrocytes Controlling Action Potentials. The Neuroscientist, 14(6) | https://doi.org/10.1177/1073858408320294
- Consecuencias neurológicas del VIH y el SIDA | NINDS Español – Última consulta: 02/05/2023.
¿Qué es y qué estudia la neurociencia?
- Enclavedeciencia [Internet]. Madrid: RAE-FECYT; 2020 [citado 23 jun 2023]. Disponible en: https://enclavedeciencia.rae.es/neurociencia
- Hormeño L, Escobar A. Fisiopatología general. Madrid: Editorial Síntesis, S.A.; 2016.
- Lorenzo MI, Simón F, Gómez-Aguado F, et al. Fisiopatología general. Barcelona: Editorial Altamar, S.L.; 2022.
- National Institutes of Health [Internet]. Rockville: U.S. Department of Health and Human Services; c1962 – 2019 [actualizado 17 oct 2019]. Sobre la neurociencia [aprox. 1 pantalla]. Disponible en: https://espanol.nichd.nih.gov/salud/temas/neuro/informacion
- National Institutes of Health [Internet]. Rockville: U.S. Department of Health and Human Services; c1962 – 2019 [actualizado 17 oct 2019]. ¿Cuáles son las partes del sistema nervioso? [aprox. 2 pantallas]. Disponible en: https://espanol.nichd.nih.gov/salud/temas/neuro/informacion/partes
- National Institutes of Health [Internet]. Rockville: U.S. Department of Health and Human Services; c1962 – 2019 [actualizado 17 oct 2019]. ¿Qué hace el sistema nervioso? [aprox. 1 pantalla]. Disponible en: https://espanol.nichd.nih.gov/salud/temas/neuro/informacion/funciones
- National Institutes of Health [Internet]. Rockville: U.S. Department of Health and Human Services; c1962 – 2019 [actualizado 17 oct 2019]. ¿Cuáles son algunas de las diferentes áreas de la neurociencia? [aprox. 1 pantalla]. Disponible en: https://espanol.nichd.nih.gov/salud/temas/neuro/informacion/areas
- National Institutes of Health [Internet]. Rockville: U.S. Department of Health and Human Services; c1962 – 2019 [actualizado 17 oct 2019]. ¿Por qué los científicos deberían estudiar neurociencia? [aprox. 1 pantalla]. Disponible en: https://espanol.nichd.nih.gov/salud/temas/neuro/informacion/estudiar
Cambiar nuestro cerebro es posible
- Sanders, R. (2017, 18 de julio) Marian Diamond, known for studies of Einstein´s brain, diez at 90. Berkeley News.https://news.berkeley.edu/2017/07/28/marian-diamond-known-for-studies-of-einsteins-brain-dies-at-90/
- Moreno-Jiménez, E.P., Flor-García, M., Terreros-Roncal, J. et al. Adult hippocampal neurogenesis is abundant in neurologically healthy subjects and drops sharply in patients with Alzheimer’s disease. Nat Med 25, 554–560 (2019). https://doi.org/10.1038/s41591-019-0375-9
- Deppermann, S., Storchak, Fallgater, A.J. et al. Stress. Induced neuroplasticity: (Mal)adaptation to adverse life events in patients with PTSD – A critical overview. Neuroscience 283, 166-177 (2014)
- Merz EC, He X, Noble KG. Pediatric Imaging, Neurocognition, and Genetics Study. Anxiety, depression, impulsivity, and brain structure in children and adolescents. Neuroimage Clin. 2018 jul 24; 20:243-251. doi: 10.1016/j.nicl.2018.07.020. PMID: 30094172; PMCID: PMC6080576.
- Gulyaeva NV. Molecular Mechanisms of Neuroplasticity: An Expanding Universe. Biochemistry (Mosc). 2017 Mar;82(3):237-242. doi: 10.1134/S0006297917030014. PMID: 28320264.
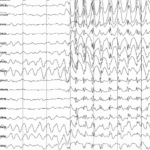
¿Qué puede aportar la electroencefalografía en los estados alterados de consciencia y daño cerebral adquirido?
- Curley, W. H., Forgacs, P. B., Voss, H. U., Conte, M. M., & Schiff, N. D. (2018). Characterization of EEG signals revealing covert cognition in the injured brain. Brain, 141(5), 1404-1421. https://doi.org/10.1093/brain/awy070
- Goldfine, A. M., Victor, J. D., Conte, M. M., Bardin, J. C., & Schiff, N. D. (2011). Determination of awareness in patients with severe brain injury using EEG power spectral analysis. Clinical Neurophysiology, 122(11), 2157-2168. https://doi.org/10.1016/j.clinph.2011.03.022
- Lechinger, J., Bothe, K., Pichler, G., Michitsch, G., Donis, J., Klimesch, W., & Schabus, M. (2013). CRS-R score in disorders of consciousness is strongly related to spectral EEG at rest. Journal of Neurology, 260(9), 2348-2356. https://doi.org/10.1007/s00415-013-6982-3
- Thibaut, A., Schiff, N., Giacino, J., Laureys, S., & Gosseries, O. (2019). Therapeutic interventions in patients with prolonged disorders of consciousness. The Lancet Neurology, 18(6), 600-614. https://doi.org/10.1016/S1474-4422(19)30031-6
- Quezada García, M. Y., Huete García, A. & Bascones Serrano, L. M (2019). Las personas con Daño Cerebral Adquirido en España. FEDACE
Priones, un nuevo punto de vista para dar luz a la enfermedad de Alzheimer
- Ashe, Karen H., y Adriano Aguzzi. «Prions, Prionoids and Pathogenic Proteins in Alzheimer Disease». Prion 7, n.o 1 (enero de 2013): 55-59. https://doi.org/10.4161/pri.23061.
- Braak, Heiko, y Eva Braak. «Staging of Alzheimer’s Disease-Related Neurofibrillary Changes». Neurobiology of Aging 16, n.o 3 (mayo de 1995): 271-78. https://doi.org/10.1016/0197-4580(95)00021-6.
- Braak, Heiko, Irina Alafuzoff, Thomas Arzberger, Hans Kretzschmar, y Kelly Del Tredici. «Staging of Alzheimer Disease-Associated Neurofibrillary Pathology Using Paraffin Sections and Immunocytochemistry». Acta Neuropathologica 112, n.o 4 (octubre de 2006): 389-404. https://doi.org/10.1007/s00401-006-0127-z.
- Castellani, Rudy J., Raj K. Rolston, y Mark A. Smith. «Alzheimer Disease». Disease-a-Month 56, n.o 9 (septiembre de 2010): 484-546. https://doi.org/10.1016/j.disamonth.2010.06.001.
- Fornari, Sveva, Amelie Schäfer, Mathias Jucker, Alain Goriely, y Ellen Kuhl. «Prion-like Spreading of Alzheimer’s Disease within the Brain’s Connectome». Journal of The Royal Society Interface 16, n.o 159 (31 de octubre de 2019): 20190356. https://doi.org/10.1098/rsif.2019.0356.
- Fraser, Paul E. «Prions and Prion-like Proteins». Journal of Biological Chemistry 289, n.o 29 (julio de 2014): 19839-40. https://doi.org/10.1074/jbc.R114.583492.
- Prusiner, Stanley B. «Novel Proteinaceous Infectious Particles Cause Scrapie». Science 216, n.o 4542 (9 de abril de 1982): 136-44. https://doi.org/10.1126/science.6801762.
- Stelzmann, Rainulf A., H. Norman Schnitzlein, y F. Reed Murtagh. «An English Translation of Alzheimer’s 1907 Paper, Über Eine Eigenartige Erkankung Der Hirnrinde». Clinical Anatomy 8, n.o 6 (1995): 429-31. https://doi.org/10.1002/ca.980080612.
- Walker, Lary C. «Prion-like Mechanisms in Alzheimer Disease». En Handbook of Clinical Neurology, 153:303-19. Elsevier, 2018. https://doi.org/10.1016/B978-0-444-63945-5.00016-7.
La neurociencia detrás de la reproducción estacional de las ovejas
- Chemineau, P., Bodin, L., Migaud, M., Thiéry, J., y Malpaux, B. (2010). Neuroendocrine and Genetic Control of Seasonal Reproduction in Sheep and Goats. Reproduction in Domestic Animals, 45, 42–49. doi: 10.1111/j.1439-0531.2010.01661.x
- Goodman, R. L., Jansen, H. T., Billings, H. J., Coolen, L. M., y Lehman, M. N. (2010). Neural Systems Mediating Seasonal Breeding in the Ewe. Journal of Neuroendocrinology, 22(7), 674-681. doi: 10.1111/j.1365-2826.2010.02014.x
- Hanon, E. A., Lincoln, G. A., Fustin, J.-M., Dardente, H., Masson-Pévet, M., Morgan, P. J., y Hazlerigg, D. G. (2008). Ancestral TSH Mechanism Signals Summer in a Photoperiodic Mammal. Current Biology, 18(15), 1147–1152. doi: 10.1016/j.cub.2008.06.076
- Ikegami, K., y Yoshimura, T. (2016). Comparative analysis reveals the underlying mechanism of vertebrate seasonal reproduction. General and Comparative Endocrinology, 227, 64–68. doi: 10.1016/j.ygcen.2015.05.009
- Singh, S. R., Hileman, S. M., Connors, J. M., McManus, C. J., Coolen, L. M., Lehman, M. N., y Goodman, R. L. (2009). Estradiol Negative Feedback Regulation by Glutamatergic Afferents to A15 Dopaminergic Neurons: Variation with Season. Endocrinology, 150(10), 4663–4671. doi: 10.1210/en.2009-0432
- Yoshimura, T. (2010). Neuroendocrine mechanism of seasonal reproduction in birds and mammals. Animal Science Journal, 81(4), 403–410. doi: 10.1111/j.1740-0929.2010.00777.x